Background:
Chronic anemia has an estimated prevalence of 5.6% within the US, where 25.3% of patients with chronic kidney disease (CKD) 3-5 have anemia of chronic kidney disease according to NHANES. Anemia in CKD has long been attributed to a decrease in EPO production due to their kidney disease. While iron deficiency is treated in anemia of chronic kidney disease, other micronutrients are less commonly tested or supplemented. Zinc may be an additional micronutrient of interest in anemia of chronic kidney disease as zinc has numerous proposed mechanisms in erythropoeisis including acting as a catalyst in the iron metabolism and heme synthesis through the activity of alpha-aminolevulinic acid dehydratase enzyme. Zinc is found in the structure of the growth factor independent 1B (Gfi-1B) Zinc finger protein and GATA-1 Zinz finger transcription factor, which functions as a regulator in erythroid cell growth by modulating gene expression specific to erythroid series including the SMAD pathways and TGF-β signaling. The interaction with zinc in signaling cascades such as the growth hormone and insulin-like growth factor-1 pathways also result in increased erythropoietin transcription and therefore increased erythropoiesis. In addition, zinc is regarded as an important erythroid differentiation factor which progress maturation of erythrocytes. Zinc has also shown to stimulate EPO production in nephrectomized rats and Zinc supplementation increased reticulocyte production in human subjects.
This descriptive, retrospective study describes zinc deficient patients with CKD 3-5 and chronic anemia; who underwent oral zinc supplementation, and their changes in hemoglobin (HGB) over a 12 month period in an academic outpatient hematology clinic in California, United States of America.
Objectives:
Primary endpoints: determine the rate of anemia resolution over 12 months following supplementation of zinc in patients with zinc deficiency, CKD, and anemia of chronic kidney disease.
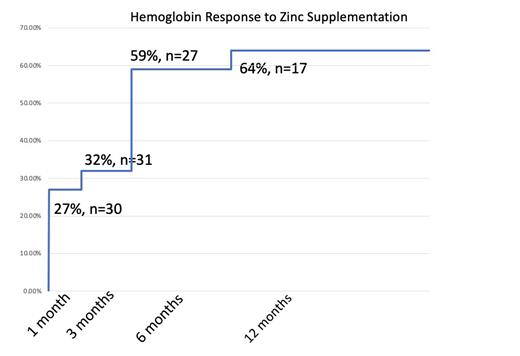
Secondary endpoints: determine if zinc supplementation in zinc deficient patients with chronic anemia and CKD 3-5 will improve HGB by at least 1.0 g.dL by 1, 3, 6, and 12 month time points.
Methods:
Hematology patients from Loma Linda University Cancer Center over the age of 18 who had CKD 3 or above (GFR <59 ml/min) with chronic anemia (HGB <12 for women, HGB <13 for men for >3 months) were identified to have zinc deficiency (plasma zinc concentration <65 ug/dL). Patients did not start new treatment for their anemia, including initiating new treatments for malignancy 3 months preceding, and within the data collection period. Patients were supplemented with Zinc Sulfate 50 mg daily and their HGB was followed over 12 months.
A retrospective analysis was completed for prior medical history, lab data, and hemoglobin was tabulated at the time markers of 1, 3, 6, and 12 months following initiation of zinc supplementation. ANOVA, Wilcoxon rank-sum, and unpaired Students and t tests were performed to determine significant differences. p <0.05 is considered statistically significant.
Results
Thirty-Four patients were identified to have CKD 3-5 with chronic anemia and zinc deficiency. They were found to have no statistically significant baseline characteristics, hematologic values at time of diagnosis, or micronutrient and hormonal etiologies for anemia. HGB prior to supplementation averaged 9.96 g/dL, WBC averaged 5.8, and PLTS averaged 149. Following supplementation HGB at 1 month average was 10.47 g/dL (p=0.19 n=30), at 3 months average of 10.49 (p=0.12 n=31), at 6 months average of 11.03 (p=0.011 n=27), at 1 year 10.93 (p=0.03, n=17).
Primary endpoint of HGB resolution was found in 12 of the 34 patients (35%). Secondary endpoint of HGB improvement by at least 1.0 g/dL was reached in 27% of patients at 1 month, 32% of patients at 3 months, 59% of patients at 6 months and 64% of patients at 12 months.
Conclusions:
Zinc supplementation improved patients' anemia with resolution of anemia in 35% of patients with incremental improvement in HGB over a 1 year time frame. There was statistically significant improvement from baseline HGB at the 6 and 12 month time markers. Further study is warranted to determine the specific mechanism of zinc deficiency in anemia with chronic kidney disease, as well as clinical studies determining zinc supplementation doses, monitoring, and toxicity.
Disclosures
Akhtari:Janssen: Speakers Bureau; Takeda: Speakers Bureau; Jazz Pharmaceuticals: Speakers Bureau; CTI BioPharma Corp., a Sobi company: Speakers Bureau; PharmaEssentia: Speakers Bureau; Sanofi: Speakers Bureau; Ispen: Speakers Bureau; SrcuraBio: Speakers Bureau; Incyte: Speakers Bureau; AbbVie: Honoraria; Amgen: Research Funding; Rigel: Speakers Bureau.